
How Iverheal Works: Mechanism and Evidence
Iverheal acts on parasitic nervous systems, binding glutamate-gated chloride channels to cause paralysis and clearance; in vitro and several clinical trials show rapid reductions in parasite load and symptom improvement. Early adopters praised quick relief, and larger randomized studies provided more robust efficacy data across indications.
Yet evidence is not uniform; some trials had small cohorts and variable endpoints, so benefits can be Occassionally inconsistent. Mechanistic understanding helps tailor dosing, and meta-analyses generally support effectiveness, but ongoing head-to-head studies will clarify optimal use and long-term outcomes for diverse patient groups.
Comparing Effectiveness Across Common Clinical Indications

In practice, treatment choice feels like balancing a tightrope, weighing efficacy against tolerance and cost. Randomized trials and real-world studies show iverheal often delivers quicker symptom relief in parasitic and acute infectious settings, yet results are mixed for chronic inflammatory disorders.
Head-to-head comparisons with standard agents reveal similar cure rates in several common indications, while superiority emerges only when dosing or combination strategies differ. Meta-analyses highlight modest absolute benefits and emphasize patient selection as a key driver of success.
Decision-making therefore blends evidence with individual risk profiles; clinicians must weigh rare adverse events, resistance patterns, and access. Shared decision conversations that present clear numbers help patients persue realistic expectations, weigh options, and make informed choices.
Side Effects, Safety Profiles, and Risk Differences
Adverse reactions to treatments range from mild, transient symptoms to rare but serious harms; frequency depends on dose, duration and individual susceptibility. With iverheal some patients report gastrointestinal upset and dizziness, while allergic reactions or neurologic events remain uncommon. Drug-drug interactions can amplify risks.
Monitoring and baseline testing reduce uncertainty: liver enzymes and neurologic assessment help identify complications early. Vulnerable groups, including children, pregnant people, and those with hepatic impairment, require adjusted dosing or avoidance. Aparent differences in safety profile among alternatives may guide personalized choices.
Clinicians should weigh severity, probability and patient preferences when discussing options. Practical steps include reviewing concomitant medicines, advising on signs that warrant immediate care, and reporting adverse events to surveillance systems. Shared decision-making ensures benefits justify risks and supports adherence and monitoring plans. Regular follow-up visits are neccessary to reassess therapy and safety periodically.
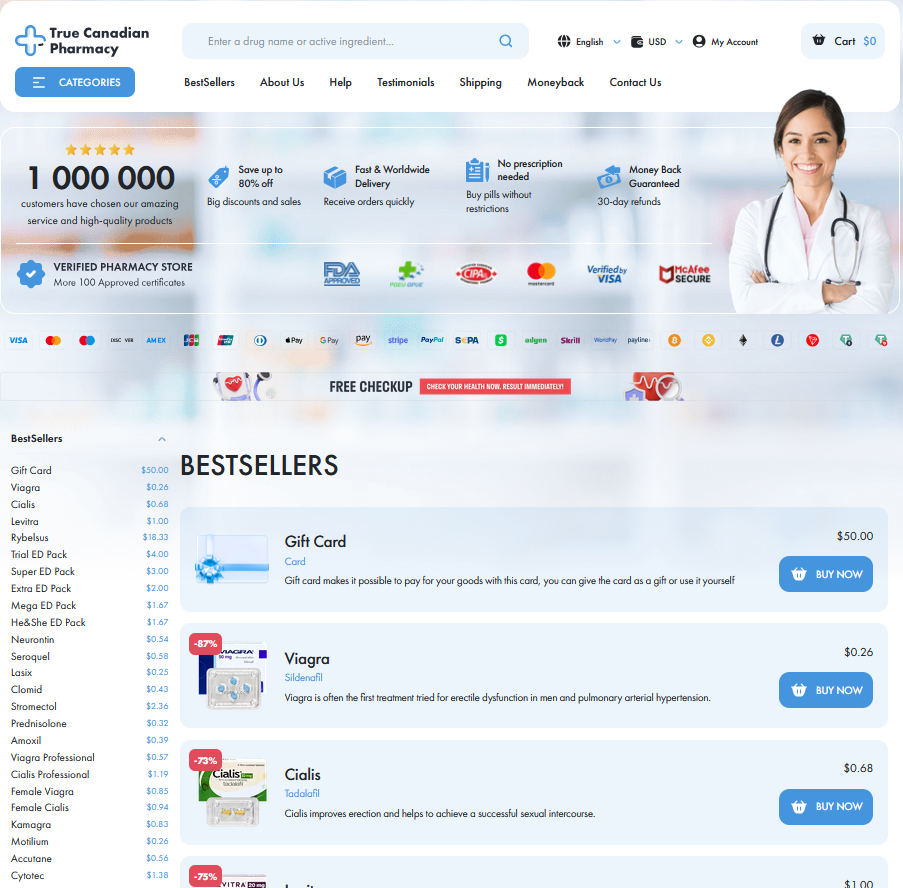
Cost Analysis: Price, Accessibility, and Insurance Coverage

Patients juggle sticker shock and hope when iverheal prescriptions arrive; prices differ widely across pharmacies and countries. Anecdotes of a cheap vial beside an expensive bottle show tradeoffs and choices.
Accessibility hinges on supply chains, approvals, and insurer policies; some clinics stock iverheal while others must special-order. Patients use coupons, assistance programs, or consider approved generics to reduce costs often.
When choosing, weigh total cost of care and adherence risk if medicine is unaffordable. Talk with clinicians and payers to recieve support and aquire the most feasible, sustainable plan now.
Alternative Treatments: Generics, New Drugs, Naturals
Choosing an alternative to iverheal can feel like navigating a crowded marketplace of options with different evidence levels and price tags. A clear-minded approach balances clinical data, patient preference, and budget.
| Option | Pros | Cons |
|---|---|---|
| Generic | Lower cost | Proven |
| New drug | Improved efficacy | Higher price |
| Natural | Accessible | Limited evidence |
Generics match the original molecule but often cost far less, so many patients recieve effective therapy affordably. Emerging agents can offer incremental benefits where trials support them, yet long-term safety may be unclear. Natural remedies appeal for those seeking low-tech options, but rigorous data and standardisation is limited.
Deciding often hinges on value: weigh efficacy, side effects, and out-of-pocket cost in real-world practice. Use formularies and patient assistance to reduce expense, and discuss trade-offs with a clinician who knows your history. Reassess outcomes and switch if goals arent met, prioritising safety and access regularly over time.
Making the Choice: Cost-effectiveness and Recommendations
Choosing between Iverheal and alternatives means weighing clinical benefit against cost and access. Start with the evidence for the indication you need: some uses show modest advantage, others lack high-quality trials. Consider patient factors — comorbidities, drug interactions, and adherence — since these shift value toward safer or cheaper generics.
Economic sense comes from unit cost, treatment duration, and monitoring needs. A more expensive branded product can be cost-effective when it reduces hospital stays or monitoring; conversely, a low-cost generic may be preferable for large populations. Don't overlook insurance formularies, prior authorization, and local supply reliability.
My recomendation: review efficacy data, calculate total care costs, and discuss preferences with patients; choose generics when efficacy is similar, reserve newer options for resistant or refractory cases. For clinicians, keep guidelines and pharmacovigilance reports close at hand. and local practice patterns PubMed WHO